The word frail originates from the French word frêle, meaning ‘of little resistance’, and from the Latin word fragilis, meaning ‘easily broken’. In clinical medicine, frailty is considered one of the significant debilitating medical syndromes commonly associated with ageing and chronic disease that implies a multifactorial decrease in physiological reserve to withstand biological stressors.1 Frailty is thought to be caused by multisystem dysregulations, chronic inflammation, cachexia and sarcopenia, resulting in an increased risk of morbidity and mortality.2
It is estimated that in the UK, the prevalence of frailty in the general population is 8.5% in women and 4.1% in men.3 In the diseased state, mortality risk generally increases with age.4 However, this risk is not uniform and the concept of frailty can be used to describe the heterogeneity of increased risk in people of the same age.5 Frailty is also important in explaining some of the differences in disease presentation. For example, in a fit individual, a heart attack commonly presents with classic cardiac chest pain, while in the frail individual this presentation is less common and being generally unwell or newly confused is more frequent.6
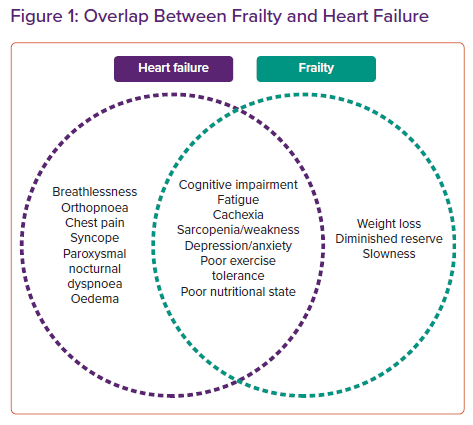
Heart failure (HF) is a global cause of morbidity and mortality with an estimated 5.7 million cases in the US alone.7 There is substantial and rapidly growing interest at the intersection between frailty and HF, as it has been shown that frailty is a powerful marker of poor prognosis and marker of outcome in the HF population.8–11 Indeed, there exists significant phenotypic and symptomatic overlap between both conditions (Figure 1). Furthermore, up to 44.5% of HF patients were considered frail using contemporary measures in a 2017 meta-analysis.12 This is independent of age or New York Heart Association classification.13 The significant bidirectional relationship between frailty and HF is evidenced by the fact that HF patients are 600% more likely to be frail and patients with frailty have a significant increased risk of developing HF.14,15 Furthermore, patients with both conditions are often more complex and have a greater burden of other comorbidities including – but not limited to – chronic obstructive pulmonary disease, chronic kidney disease, dementia and anaemia.1,11,16
Interestingly, frailty appears to be much more common in HF with preserved ejection fraction (HFpEF) than in HF with reduced ejection fraction (HFrEF).17 This is likely to be secondary to the fact that HFpEF patients typically suffer a great burden of comorbidities compared to the HFrEF population.17 Furthermore, HFpEF patients are more likely to suffer non-cardiac hospitalisations.17 Finally, frailty is more likely to be present in those who present to hospital with acute decompensation than in well-compensated community HF patients.18
The focus of this article is to review the literature with regards to HF and frailty. Specifically, this article will focus on the pathophysiology of frailty, its assessment in HF and its prognostic implications.
Pathophysiology of Frailty
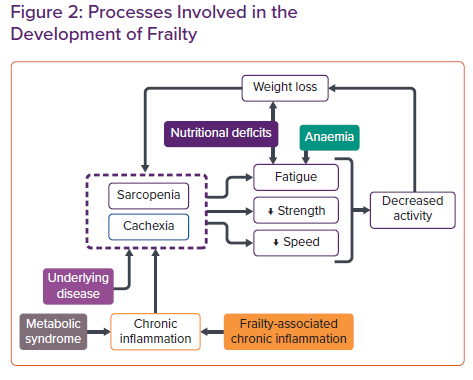
The physiological processes involved in the development of frailty syndrome are predominantly of an immune, endocrine and musculoskeletal nature resulting in a reduction in strength, endurance or cognitive function (Figure 2).19–21
Inflammatory pathways have been elucidated as an important mechanism in the development of frailty syndrome.22,23 Population-based studies have linked elevated levels of the proinflammatory cytokine interleukin-6 to frailty in both community and inpatient populations in addition to identifying higher serum levels of C-reactive protein, tissue necrosis factor-α, and white blood cells in frail members of community and inpatient populations aged ≥70 years.22,24,25 Additionally, lower levels of the negative acute phase reactant albumin correlate with a higher degree of frailty in inpatients aged >75 years.22
Nutritional deficits have also been implicated in the pathophysiology of frailty, with frail patients more likely to have multiple nutritional deficits than non-frail patients.25 High protein intake appears to be protective against frailty in older populations and, conversely, low protein intake has been associated with higher frailty risk.26,27 Micronutrient deficits are also associated with frailty risk, with low intake of vitamins D, E and C, and folate being associated with frailty independent of total calorie intake.26 Vitamin B12 deficiency has also been identified as more common in pre-frail or frail individuals when compared with a non-frail population.28 Healthier diets, such as the Mediterranean diet and high fruit and vegetable intakes, have been associated with decreased risk of frailty in meta-analyses.29,30
Finally, the development of anaemia has been identified as a contributing factor to frailty syndrome. Anaemia is more prevalent amongst frail populations and haemoglobin levels negatively correlate with frailty risk.31–33 The anaemia identified in frail patients is commonly found to be normocytic, with haemoglobin levels inversely correlated with interleukin-6, suggesting an interplay between anaemic and inflammatory pathological processes in the development of frailty syndrome.32
Once established, the phenotypical characteristics of frailty feed into each other, leading to a downward spiral in which the patient is perpetually becoming increasingly frail. Key to this cycle are the processes of sarcopenia and cachexia. These conditions often overlap but have distinct definitions. Sarcopenia is typically defined by low muscle mass and function, while cachexia is defined as weight loss in the presence of underlying illness, with chronic inflammation identified as a key pathophysiological mechanism.34,35 Considering the prevalence of markers of chronic inflammation seen in frailty patients, it can be assumed that cachexia plays a role in the pathological cycle amongst a significant proportion of patients with frailty. Figure 1 illustrates the role of abnormal physiology in the cycle of frailty progression, with reference to Fried’s cycle of frailty.36
Identifying Frailty in Heart Failure
The assessment of frailty in the HF patient is challenging because of the lack of a universal, easily used set of diagnostic criteria or screening tool. While the term ‘frailty syndrome’ was first described in 1991 in a landmark paper,and has since been adopted into clinical practice and the research environment, as of 2021, there is still no internationally agreed definition or diagnostic criteria.37 Furthermore, frailty is widely recognised and used by the general clinician in guiding treatment decisions and estimating prognosis. This recognition is often performed using a superficial ‘eyeball test’ or the ‘end-of-the-bed-o-gram’ rather than a validated frailty risk assessment. This is because the most well-validated tools can often be cumbersome and resource-intensive in routine medical practice.
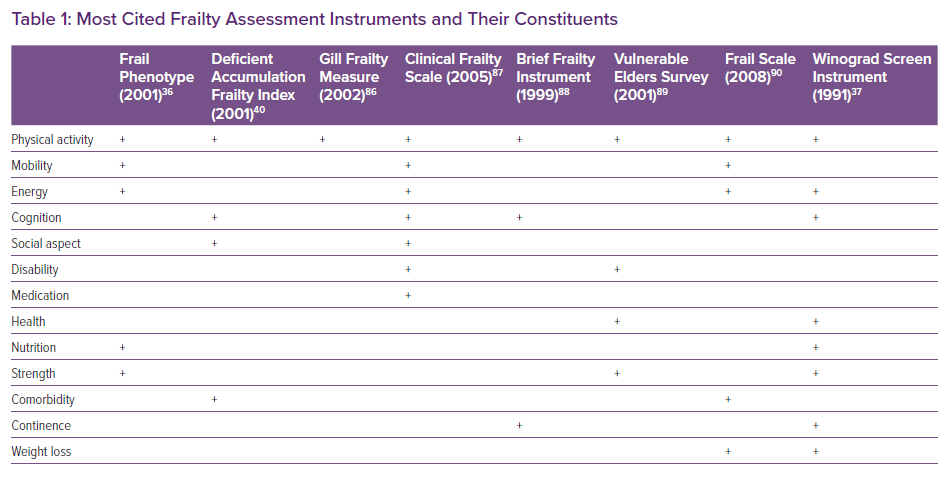
Generally, frailty assessment tools are derived from two basic concepts in frailty: a unidimensional/physical model that views frailty as a physical problem, and a multidimensional/holistic model that incorporates both physical problems as well as psychological and social problems.38,39 In a recent review, 67 frailty measurement instruments were identified, and these often-exhibited significant heterogeneity with regards to which parameters were used.40 Table 1 shows the nine most cited frailty assessment tools identified from this review and their individual constituents.40
The frail phenotype/Fried scale is the single most commonly used and validated tool in the cardiovascular disease (CVD) population.36 This was first described over two decades ago and subsequently validated in the in the Women’s Health and Aging study.36,40 The Fried scale consists of five domains: unintentional weight loss, weakness as measured by hand grip strength, self-reported exhaustion, a slow gait speed and low self-reported physical activity. Frailty is defined as three or more criteria being present, and pre-frailty as two or more. The presence of frailty as measured on the Fried scale has been demonstrated with worse clinical outcomes and a greater functional impairment in both the HF and non-HF population.41,42 Fried’s criteria is the most used tool to measure frailty, but it can be limited by capturing only the physical frailty, and the requirement for a dynamometer precludes its use without special equipment. Finally, in the context of diuresis it is difficult to accurately assess unintentional weight loss.
The deficient accumulation frailty index is another commonly used frailty tool often used in the CVD population.43 It sums the total number of impairments a patient has during their activities of daily living, comorbid conditions, and abnormal laboratory values. Frailty index categorises the individuals in a quantitative continuum rather than an absolute and can often be assessed from medical records. The disadvantages of this assessment tool are that it is time consuming in routine use and its reliance of the number of deficits rather than the nature of the deficit. Therefore, in certain circumstances it may overestimate the frailty burden.
While a variety of frailty measures and scores have been used in HF, none have been developed and validated in this cohort. These patients are more difficult to assess using contemporary frailty scores for multiple reasons including, but not limited to, the significant overlap between frailty and HF, and the inference of frailty with possible HF treatment. The need for a HF frailty assessment tool prompted the Heart Failure Association of the European Society of Cardiology (ESC) to release a position paper in 2019 on frailty in HF, defining frailty and creating a foundation (based on clinical, psycho-cognitive, functional, and social domains) for the design of a tailored validated score in the HF patient.44,45
Prognostic Implications of Frailty in Heart Failure Patients
While there is no single validated frailty assessment tool in the HF population, there is still considerable evidence demonstrating that frailty and its components are correlated with worse HF outcomes. Hand grip strength has consistently been found to be an independent predictor of survival in the HF population, with higher grip strength corresponding with increased survival.46 In a meta-analysis in >2,300 patients with CVD including HF, lower hand grip strength was associated with increased risk of CVD death, all-cause mortality, and admission for HF.47 Poor lower-extremity function at baseline, measured by gait speed or functional assessments such as the 6-minute walk test (6MWT) or the short physical performance battery, has also been associated with increased all-cause and HF mortality.48,49
Additionally, HF patients with decreased gait speed or poorer lower extremity function at follow-up are at higher risk of all-cause mortality when compared with HF patients who maintain gait speed or lower extremity function.48 Higher gait speed or better lower-extremity performance at baseline have also been demonstrated to reliably predict a lower risk of all cause and HF hospitalisation, with improvement in lower-extremity performance or gait speed at follow up reducing risk of all-cause hospitalisation further.48,50,51 Self-reported exhaustion/fatigue is an important component of the frailty phenotype. Fatigue is more challenging to measure objectively, therefore research into its relationship with HF is more limited. However, it has been demonstrated that greater levels of fatigue are linked with worse clinical outcomes after controlling for other prognostic variables.52 Cognitive impairment is a commonly cited feature on many frailty assessment scales and is more prevalent in the HF population, and has been associated with increased hospitalisation in HF patients.53,54
Despite the perceived issues with identifying an existing frailty assessment tool for use in estimating HF prognosis, there have been efforts to validate existing frailty assessments tools for this purpose. Boxer et al. categorised 60 HF patients into three groups based on the frailty phenotype status where the frail patients had the highest mortality at follow-up compared to their counterparts.55 Similarly, in the study by Madan et al. in 40 HF patients, frailty was associated with increased combined endpoint of mortality and all-cause hospitalisation.56 McNallan et al. investigated the relationship between frailty and mortality in HF patients using a the deficit model and a modified version of Fried’s frailty phenotype, differing in patient assessment by using the physical component score of the Short Form 12 health questionnaire as a surrogate for both strength and speed.57,58 This demonstrated that in HF patients defined as frail, the risk of mortality was doubled (HR 2.04; 95% CI [0.99–4.18]). Tanaka et al. demonstrated that frailty is independently associated with worse clinical outcomes irrespective of age, BMI, ejection fraction and gender.59
In the advanced HF population awaiting a heart transplant, frailty was found to be an independent predictor of all-cause mortality.60 Furthermore, this finding was replicated in patients with HF following CRT with the implication that frailty is an independent predicator of response to CRT.61 In the left ventricular assist device (LVAD) population HF has repeatedly been demonstrated to independently predict outcomes.62,63 Furthermore, in patients with sarcopenia undergoing LVAD therapy, there was a general trend towards increasing hospital stay and mortality.64
In summary, there is significant evidence that both the individual components of frailty and various definitions of frailty as a syndrome can be used to predict prognosis in HF patients.
Management Implications in the Frail Heart Failure Patient
Frailty adds an increasing layer of complexity to the management of the already complex HF patient. Frailty also leaves patients more at risk from guideline-directed medical therapy because of their increased vulnerability to adverse drug effects, such as hypotension and subsequent falls. Therefore, the management of the frail HF patient involves more pragmatism and less rigorous adherence to guidelines. Furthermore, frail patients are more likely to benefit from non-pharmacological interventions than their non-frail counterparts. There are currently two broad categories of intervention for the frail HF patient: exercise and physical rehabilitation and diet and nutritional strategies.
Exercise and Physical Rehabilitation
The 2021 ESC HF guidelines suggest that supervised, exercise-based cardiac rehabilitation programmes should be offered to patients who are frail or with multiple comorbidities. This is based on a class IIa level of evidence.65 Exercise programmes are a promising intervention in frail HF patients as there is evidence of dual benefit, addressing both a patient’s cardiac failure and frailty simultaneously. For HF patients, the positive impact of exercise on physical function, quality of life and exercise capacity is well documented.66–68 Despite these benefits, uncertainty still exits regarding the overall impact on mortality and HF hospitalisations.69,70 Intense exercise therapy has shown that it may improve peak oxygen consumption (VO2).71 Furthermore, exercise training has been shown to reduce serum markers of inflammation in HF patients, suggesting a reduction in the chronic inflammation that acts as a key pathophysiological process in both HF and frailty.72,73 Inflammation may also play a role in predicting benefit from exercise training, as HF patients with higher baseline levels of inflammatory biomarkers have been noted to show poorer improvements in peak VO2 as a result of exercise training when compared with HF patients with lower baseline inflammatory biomarkers.74
Diet and Nutrition Strategies
Dietary support in frailty aims to address the numerous nutritional deficits seen in frail patients. Micronutrient deficiencies common in frailty include vitamins D, E, A, B12, thiamine, iron and folate.75 Long-term vitamin D supplementation in the advanced HF patient has not been demonstrated to reliably improve outcomes or cause harm.76 Thiamine supplementation has been found to be ineffectual in impacting HF progression or physical performance, and while folate supplementation has shown promise in lowering N-terminal pro-brain natriuretic peptide levels, the evidence for this is limited and there is no evidence of clinical benefit in HF populations.77,78 The evidence for micronutrient supplementation (calcium, magnesium, zinc, copper, selenium, thiamine, riboflavin, folate, vitamins A, B6, B12, C, E, D and coenzyme Q10) is mixed and inconclusive.79,80 Iron replacement in the frail HF patient has a strong evidence base and patients should be regularly screened and treated.65
With regards to macronutrients, high-calorie, high-protein diets in HF patients with significant unintended weight loss have been demonstrated to improve quality of life and 6MWT performance.81 Supplementation with essential amino acids has been shown to improve peak VO2 and 6MWT performance in muscle-depleted HF patients but did not increase muscle mass.82 Conversely, supplementing resistance exercise with branched chain amino acids in HF patients led to no additional improvement in strength or VO2 max when compared with HF patients undertaking exercise without supplementation.83
The future of nutritional support in frail HF patients may lie in a patient-personalised approach. In a clinical trial of 120 malnourished patients hospitalised with HF, personalised nutritional interventions delivered over a 6-month period led to decreased all-cause mortality (20.3% versus 47.5%; HR 0.37; 95% CI [0.19–0.72]; p=0.003), cardiovascular mortality (16.9% versus 42.6%; HR 0.35; 95% CI [0.17–0.72]; p=0.004) and re-admission for HF (10.2 versus 36.1%; HR 0.21; 95% CI [0.09–0.52]; p=0.001).84 Taken together, this suggests that nutritional treatments of frailty in HF should be tailored to the individual patient’s nutritional needs, with or without micronutrient supplementation where appropriate. Further research is required to assess the impact of personalised nutritional support in non-malnourished frail HF patients.
The Role of the Multispecialty Multidisciplinary Team in Heart Failure Management
Recent evidence from Liverpool, UK, has shown that a multispecialty multidisciplinary team approach provides seamless integration of primary care community services with secondary and tertiary care.85 The multispecialty team consists of HF specialists (consultants, specialist nurses), along with a geriatrician, renal physician, diabetes specialist, chest physician, pharmacist, pharmacologist and palliative care physician. This approach allows for consensus decisions from multidisciplinary team meetings, providing a holistic approach for HF patients with comorbidities, polypharmacy and frailty. This approach can also reduce hospitalisations and inconvenience to patients by preventing the need to attend multiple specialty clinics. This model can also lead to significant cost savings to the healthcare system.
Conclusion
HF is among the high-priority challenges in the field of cardiology. Frailty represents the endpoint of a multitude of complex processes. The incidence of frailty and HF and the combination of both is increasing with an ageing population. The frail HF patient represents the most complex presentation of HF.
Routine and meaningful assessment and management of frailty in the HF patient can offer more intensive treatment to improve outcomes. These patients are likely to be more complex than their non-frail counterparts and more likely to benefit from a multidisciplinary HF team approach. Physical exercise programmes are a useful resource and are recognised in ESC HF guidelines. Further research on personalised nutritional interventions in frail HF patients is recommended to validate the promising evidence available at present. Finally, development and validation of an assessment tool to identify frailty in HF populations is recommended to facilitate delivery of multidisciplinary care to these complex patients.