Heart failure (HF) is a variable, chronic, progressive and life-limiting illness with significant impacts on quality of life (QOL), use of acute care and family and caregiver burden.1,2 Palliative care is described by the WHO as an approach that “improves the quality of life of patients and that of their families who are facing challenges associated with life-threatening illness.”3 Palliative care includes management of suffering (including physical, psychosocial and spiritual domains), communication of prognosis, assessment of prognostic awareness and advance care planning (ACP).3–5 Professional bodies now recommend the integration of palliative care into HF therapy.2,6 Significant barriers remain, including access to palliative care resulting from geographical barriers and workforce shortages.1 Telehealth is a rapidly growing means for providing palliative care.7–9 In fact, while telehealth has grown organically over the past two decades, COVID-19 has precipitated a 38-fold growth in telehealth in the US from 2020 to 2021.10 This review will describe the role of telehealth in ACP for HF, as well as the role of virtual education for training clinicians in ACP communication.
Advance Care Planning
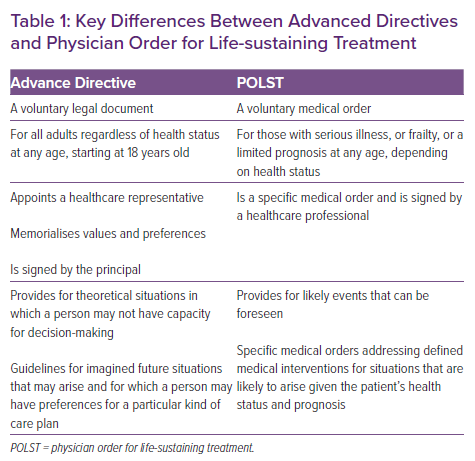
ACP includes discussions of life values, goals for treatment and the periodic revisiting of these wishes to integrate with appropriate treatment as underlying diseases advance.11,12 Communication between patients, their loved ones or decision-makers and clinicians is at the core of ACP. Because of a variety of factors, many individuals would like to control decision-making around healthcare, particularly choices at the end of life.13 The advance directive (AD) is a written, legal document that serves as a guide for a patient’s decision-makers.14 The AD developed as a result of landmark US court cases, including those of Karen Quinlan and Nancy Cruzan, regarding the ability of patients or their surrogate or representative to refuse or withdraw medical care.15,16 While prevalence varies, AD are present in North America, Europe, Australia and parts of Asia.12,16,17 These are distinct from decisions regarding resuscitation and CPR, which are transmitted in orders for life-sustaining treatment, for example the physician order for life-sustaining treatment (POLST) or do not resuscitate (DNR) orders (Table 1).12,17,18
The AD developed as a way to enact ethical principles of autonomy and individual control over the dying process, but often do not delve to the level of detail required for individualised medical care.13,15,19 A proportion of patients with AD do not have their wishes followed.13 The advent of POLST or DNR orders increased the frequency of goal-concordant care.13,18,20 However, in addition to AD and/or POLST, given the growing complexity of modern medical care and increasingly nuanced medical decision making, patient–provider communication is the mainstay of ACP.
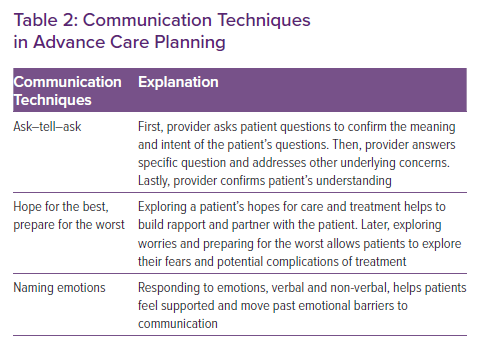
Communication for ACP has been found to be most effective when initiated by a provider well known to patients over multiple visits (Table 2).15 ACP conversations can involve discussions of prognosis, deciding surrogate decision makers, expected disease trajectories, life-sustaining treatments, interventions and procedures along with general attitudes towards care. Barriers to effective communication for ACP are numerous, and include patient and clinician hesitancy to discuss, lack of training and comfort in ACP discussions, time constraints and access to specialty palliative care.1
Advance Care Planning in Heart Failure
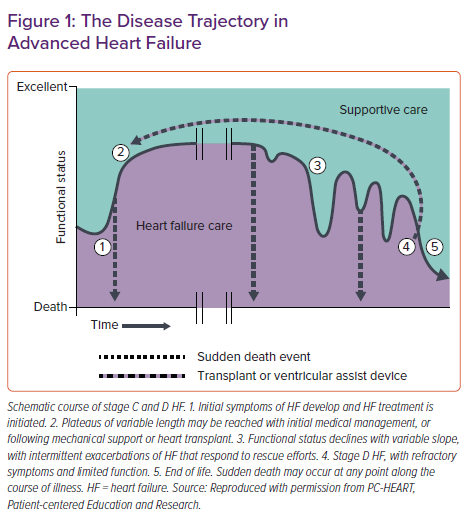
Discussion of ACP in cardiac disease and HF has grown significantly in the past two decades, but palliative care and hospice care remain underused in these populations.21,22 Previous models of ACP and communicating around serious illness centred around oncologic disease, despite the morbidity and mortality associated with HF.19 HF is the final common pathway of a variety of health conditions, each with their own illness trajectories and comorbidities, making prognostication notoriously difficult.4,23 However, because of the variability of exacerbations and decompensations, early ACP is a crucial piece of an effective intervention (Figure 1).24 In addition, assessing prognostic awareness – defined as awareness of having an incurable disease and shortened life expectancy – sets the stage for ACP conversations.5
Key decisions in HF include life-sustaining treatments (e.g. CPR, other resuscitative efforts), interventions (e.g. placement of an ICD or left ventricular assist device), level of care (e.g. transfers to hospital or an intensive care unit), and intensity of medication treatment and adverse effect management, among many others.24 ACP in advanced HF also involves discussions of deactivation (e.g. of an ICD or left ventricular assist device), ideally occurring at the time of intervention or implantation.
ACP interventions in HF show improvement in QOL and improvement in depression, but mixed findings regarding quality of death and site of death.25–27 Effective ACP interventions involve tying discussions to a significant event (e.g. following hospitalisations), multiple interventions over time, involvement of family or surrogate decision makers and participation of the multidisciplinary team.27 In ACP discussions, exploring goals and values prior to discussing particular preferences for treatment decisions leads to more effective and focused communication (Table 2). Mixed evidence quality is noted in multiple reviews because of heterogenous populations studied and small samples sizes, implying the need for additional high-quality studies.25–27
Telehealth in Heart Failure
HF care involves specialised, multidisciplinary, highly coordinated care with frequent monitoring.28,29 The growth of chronic diseases, such as HF, and the concomitant growth of personal devices creates a space for innovative technology, including telehealth.29,30 Telehealth is defined broadly as the delivery of healthcare from a distance, either provided synchronously or asynchronously.30,31 The applications of telehealth in HF are far reaching, spanning from remote patient monitoring with wearable technology to direct consultations with HF providers.29
Telehealth has many facilitators for adoption in HF. These include the provision of care to remote or under-resourced settings, patient-centred and personalised care, improved coordination of care for high-cost conditions such as HF and increased decision support for complex populations.29 Nevertheless, there are also many barriers to telehealth. These include access to personal electronics, acceptance of new technology (particularly in older people), limitations in clinician reimbursement (which received a temporary reprieve during COVID-19), lower quality of patient–provider relationships, the learning curve for staff involved and regulatory constraints.29,30,32
COVID-19 advanced the use of telehealth exponentially because of the need to rapidly reduce in-person contact for prevention of transmissible disease. However, the field had grown significantly prior to 2020 because of the facilitators listed above.30,31 Multiple studies show that telehealth is non-inferior to in-person, direct patient care for direct consultation with providers.31,33,34 Telemonitoring and structured telephone interventions reduce hospitalisations and death in HF.28,35,36 Additional findings show telemonitoring can also improve depression severity and QOL in HF.37
Telecommunication in Heart Failure: Approaches to Shared Decision-making
Telehealth interventions have the possibility of expanding the reach of palliative care in all disease entities, including HF.7,9,38–41 Given the potential benefits of palliative care and overall shortages of palliative care providers, the question arises whether telehealth is an appropriate venue for ACP communication. Studies of telehealth interventions are varied, with many focused on symptom monitoring and caregiver support in addition to ACP and serious illness communication.7,38,40 Tele-hospice care has an evidence base of >20 years and has been generally well accepted by patients, caregivers and hospice staff.42–44
COVID-19 provided a natural experiment for rapid transition to telehealth and telecommunication. Lally et al. describe that documentation of goals of care – which is tightly linked to ACP – increased with transitions to telehealth.8 In an editorial, Lee notes that a Zoom family meeting improved coordination of care and provided a patient- and family-centred approach to care.45 The frequency, intensity, and modality of effective ACP interventions are debatable.
Hoek et al. describe a weekly teleconsultation intervention for palliative care in advanced cancer patients that led to increased distress, suggested to be related to excess attention to suffering during the intervention.39 They also describe an unknown component of the possible negative effect of technology on patient’s well-being.39
ENABLE CHF-PC built on a previously-established nurse-led telehealth intervention in palliative care populations.40 Findings showed no difference in QOL and mood between intervention and usual care groups, which the authors believed to be related to higher pre-existing QOL and mood symptoms. In addition, a large percentage of participants were unable to complete the telehealth intervention and attend in-person visits, believed to be an under-‘dose’ of the intervention. While it is difficult to draw broad conclusions regarding telecommunication for ACP, telehealth interventions require selection of appropriate patients and level of intervention, particularly when discussing challenging topics.
A common theme across relevant literature for palliative care in telehealth is the challenge of attuning to interpersonal cues and non-verbal communication.8,39,41 Tips for improved communication include using verbal rather than non-verbal cues to express empathy, acknowledging the awkwardness of the medium and the loss of in-person interaction (particularly during COVID-19), positioning equipment appropriately, looking at the camera rather than the screen to approximate eye contact, and also leaving time for small-talk and rapport-building.41 It also may be appropriate to offer subsequent in-person visits or visits with interdisciplinary team members to continue conversations.
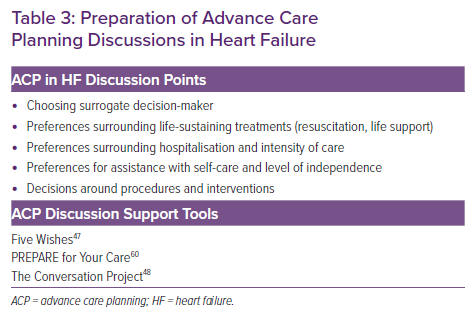
ACP conversations can occur between any member of a healthcare team and patients at any stage of health. A team-based approach helps to share the workload, using nursing and social work team members as available to prepare for the visit and follow-up with questions and resources. Pre-planning with ACP tools can help guide discussions, as well as planning to spend a visit on the topic (Table 3). In virtual care, mailing or electronic communication of these tools, as well as ACP documentation (e.g. blank advance directives) can facilitate more specific conversations. Screen-sharing capability can also help with viewing documents, such as previously completed advance directives or other ACP documentation. ACP conversations take multiple conversations and should be revisited over time.
Concerns for a digital divide based on age with moves to telehealth present a genuine challenge to ACP conversations. ACP tools such as PREPARE for Your Care have been shown to be effective for increasing ACP documentation in diverse and elderly populations.46 Other tools, such as The Conversation Project and Five Wishes, provide multiple electronic resources that can be printed and mailed or provided to patients.47,48 Other innovations include ACP group visits, which provide a space for group discussions of ACP and also increases completion of ACP documentation.49 These have migrated to virtual platforms during COVID-19 and can be an additional resource for continuing ACP conversations.
Discussion of life-sustaining treatments, including cardiopulmonary resuscitation and forms of life support, can also benefit from telehealth interventions. Regardless of the platform, discussions of resuscitation will benefit from being normalised (e.g. “I talk to all my patients about this topic”) and using clear and simple language to introduce the topic (e.g. “When the time comes that your heart and breathing stop, we can allow you to die naturally or try to revive you”). Video and virtual reality interventions providing education on life-sustaining treatments and ACP have been effective in increasing comfort with ACP and discussing ACP decisions.50,51 While there has been no comparison of virtual reality to video interventions in ACP, virtual reality is speculated to be more immersive, although this intervention was not performed in a seriously ill population and may not be generalisable.51
Virtual Clinical Education for Communication
Communication of difficult topics is at the core of ACP, regardless of the underlying diagnosis. One area of growth in the integration of palliative care in HF is communication training for cardiologists. The goals of these interventions are to improve the comfort of cardiologists in having conversations regarding serious illnesses and begin ACP earlier, potentially preventing the need for additional specialty palliative care in light of palliative care workforce shortages.52 Cardiology-specific communication training includes CardioTalk, which is a well-received adaptation of VitalTalk.53 The training is often multi day and involves standardised patients and guided communication feedback.54 Alternatives include using serious illness communication guides and training programs focused on using these guides.54
Other approaches to ACP education involve a focus on AD completion, such as completion of one’s own AD or that of a loved one.55 This approach allows participants to consider their own goals and values for medical care and encourages empathy for patients and caregivers as they embark on challenging discussions. However, this method focuses on ACP documentation and particular interventions rather than the process of eliciting goals and values for medical care. A more values-based approach for ACP education includes using conversation starter guides as a starting point for discussions (Table 3).55
Communication training sessionss similar to VitalTalk have been converted to a virtual format during COVID-19, yielding high satisfaction and comparable self-reported communication preparedness to in-person training.56 Prior to COVID-19, approaches to virtual clinical education were found to be non-inferior if they included direct communication and coaching by clinical educators.57 Wilcha describes a variety of virtual adaptations to medical education during COVID-19, with the overall finding that virtual interventions are effective.58 However, one major caveat is that students described declining mental health during the period studied, which is – in part – attributed to social isolation and fatigue with virtual platforms.
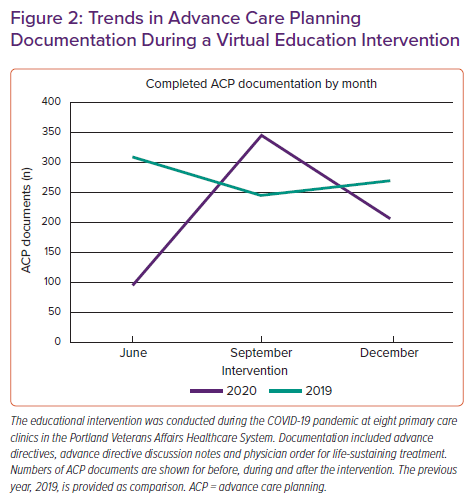
The authors of this current review performed virtual education regarding ACP during COVID-19 to eight primary care clinics in the Portland Veterans Affairs Healthcare System. This education developed out of a scarce resource allocation committee and an initiative to increase ACP discussions in the setting of COVID-19. Sessions were virtual lectures via Microsoft Teams and included physicians, advance practice providers, nurses and social workers. Given the newness of virtual platforms and limited time allotted for sessions, the authors adapted prior serious illness communication training programmes and a conversation guide developed by the authors into a 40-minute interactive case-based discussion of a man with coronary artery disease and HF. Beyond training participants in the basics of serious illness communication, we strongly encouraged completing ACP documentation given the risk of serious illness and hospitalisation with COVID-19. Documentation recommended included the AD and POLST. In addition, we encouraged completing AD discussion notes, which describe narrative discussions of ACP, and life-sustaining treatment plans, which are a Veterans Affairs approximation of POLST.59 Of note, life-sustaining treatment plans were not included in comparisons because of adoption in November 2019 by Portland Veterans Affairs Healthcare System.
Documentation of AD, POLST, and AD discussion notes spiked during the intervention (Figure 2). This is particularly impressive, given the degree of virtual care and overall decrease in patient volume seen during the autumn of 2020 compared to prior years. The decline in ACP documentation seen in December 2020 is difficult to interpret, but may imply that on-going interventions will be needed to increase ACP documentation during periods of high-volume virtual care.
Conclusion
With a globally ageing population and increasing prevalence of HF, ACP will continue to be a focus of high-quality HF management in the coming decades. ACP communication empowers patients and providers alike to focus on the goals and values that patients prioritise, and these discussions are particularly beneficial earlier in a patient’s course. The growing use of telehealth is likely to facilitate improved ACP discussions in HF, although some challenges with technology platforms may interfere with the quality of these discussions. Lastly, communication training in HF and cardiology is an emerging area of interest that will push ACP discussions upstream. Transitions to virtual communication education appear non-inferior to in-person discussions thus far. The impact of COVID-19 on all of these trends is continuously evolving, and opportunities exist to accelerate ACP in HF care via telecommunication.