Heart failure (HF) impacts all population groups, but varies based upon an individual’s race, ethnicity and sex.1 Black patients are disproportionately affected by HF compared to other groups. Black patients are diagnosed with HF at younger ages and have the highest prevalence of HF.1–3 The age-adjusted death rate for HF is highest in Black men (118.2 per 100,000), followed by non-Hispanic White men (111.3 per 100,000), Black women (86.0 per 100,000) and White women (80.4 per 100,000).4 The prevalence of HF is similar among Hispanic and White patients, but may increase in Hispanic patients since abnormal left ventricular structure/function has been observed more at younger ages in Hispanic patients than in White patients.1,5,6 Limited data exist on HF prevalence among American-Indian patients, given significant underreporting, but HF mortality rates in American-Indian women approach the rates present in White women.1,7,8
Hospitalisation for heart failure (HHF) represents a sentinel event that portends the highest risk for a poor clinical outcome and/or death. HHF rates for Black men and women are approximately two and a half times higher than White patients.2 The relative rate of HHF has improved for most racial and ethnic groups over the past decade but has not changed for Black patients.2 The mortality rate from HF has increased for Black men and women, exceeding White men and women, for adults under age 65 years.9
Many of these disparities are related to undertreatment of patients of colour. The purpose of this review is to explore the use of HF guideline-directed medical therapy (GDMT) in Black, Hispanic and American-Indian populations, examine the reasons for under-prescribing and evaluate actionable strategies to improve access to GDMT in HF among patients of colour. Proper use of GDMT may reduce existing racial and ethnic disparities in HF by improving patient symptoms, lowering the risk of HHF and reducing mortality.
GDMT in HF
GDMT at target study doses improves outcomes in HF with reduced ejection fraction (HFrEF).10 Clinical practice guidelines recommend β-blockers, angiotensin receptor-neprilysin inhibitors (ARNIs)/angiotensin-converting enzyme inhibitors (ACEIs)/angiotensin receptor blockers (ARBs), mineralocorticoid receptor antagonists (MRAs) and sodium–glucose cotransporter 2 inhibitors (SGLT2Is).10,11 A combination of hydralazine/isosorbide dinitrate with GDMT also increases survival among Black patients.12 SGLT2Is and MRAs may improve outcomes for patients with HF with preserved ejection fraction.13,14
GDMT is under-prescribed for all racial and ethnic groups. Historically, patterns of GDMT prescribing have been systematically worse among patients of colour.15,16 Get With The Guidelines Heart Failure (GWTG-HF) is a quality improvement programme designed to help hospitals optimise GDMT use. Its precursor was the Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients With Heart Failure (OPTIMIZE-HF).17,18 This programme was able to increase GDMT prescribing to similar or higher levels in African-American patients compared to patients from all other included racial and ethnic groups.19 However, the majority of GDMT was under-prescribed to all groups, with most treatments except for ACEI/ARB and β-blockers being prescribed to <50% of eligible patients.19 Due to a higher hypertension burden, target dosing of β-blockers and ARNIs is more commonly achieved among Black patients.20 In addition, Hispanic patients were less likely to receive discharge instructions.21,22 American-Indian populations are also known to be under-prescribed for cardiovascular disease treatment; underreporting limits data on HF GDMT prescribing for this group.7,8
Studies of outpatient HF populations in a national HF quality initiative showed under-prescribing of GDMT. The CHAMP-HF outpatient registry revealed that only 1% of eligible patients were simultaneously receiving target doses of ACEI/ARB/ARNI, β-blockers and MRA.20 In CHAMP-HF, Black race, higher systolic blood pressure and a history of hypertension were associated with target doses of ACEI/ARB prescription, while older age, Hispanic ethnicity, chronic renal insufficiency and higher ejection fraction were associated with lower likelihood of ARNI therapy.20 The same registry also revealed better prescribing of GDMT across most racial and ethnic groups when simultaneously prescribed with an ARNI, except for hydralazine/nitrates, which were provided to only 15% of eligible Black patients.23 Nevertheless, prescribing patterns for target dosing of ARNI and hydralazine/nitrates remained <9% for all racial and ethnic groups eligible for GDMT.23 Unfortunately these findings are similar to the underuse reported in another outpatient registry, IMPROVE-HF, 12 years earlier.24
Worldwide, there is also suboptimal uptake of GDMT. The INTERCHF study showed that rates were very low, varying from β-blocker use in only 48% of patients in Africa to 27% of patients using MRAs in southeast Asia.25
Barriers to Optimal GDMT Prescribing in HF for Black, Hispanic and American-Indian Populations
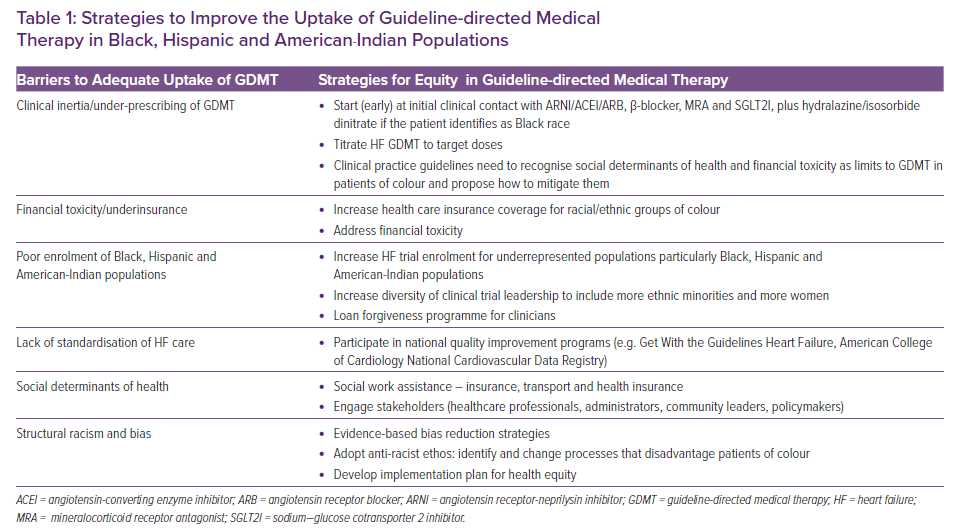
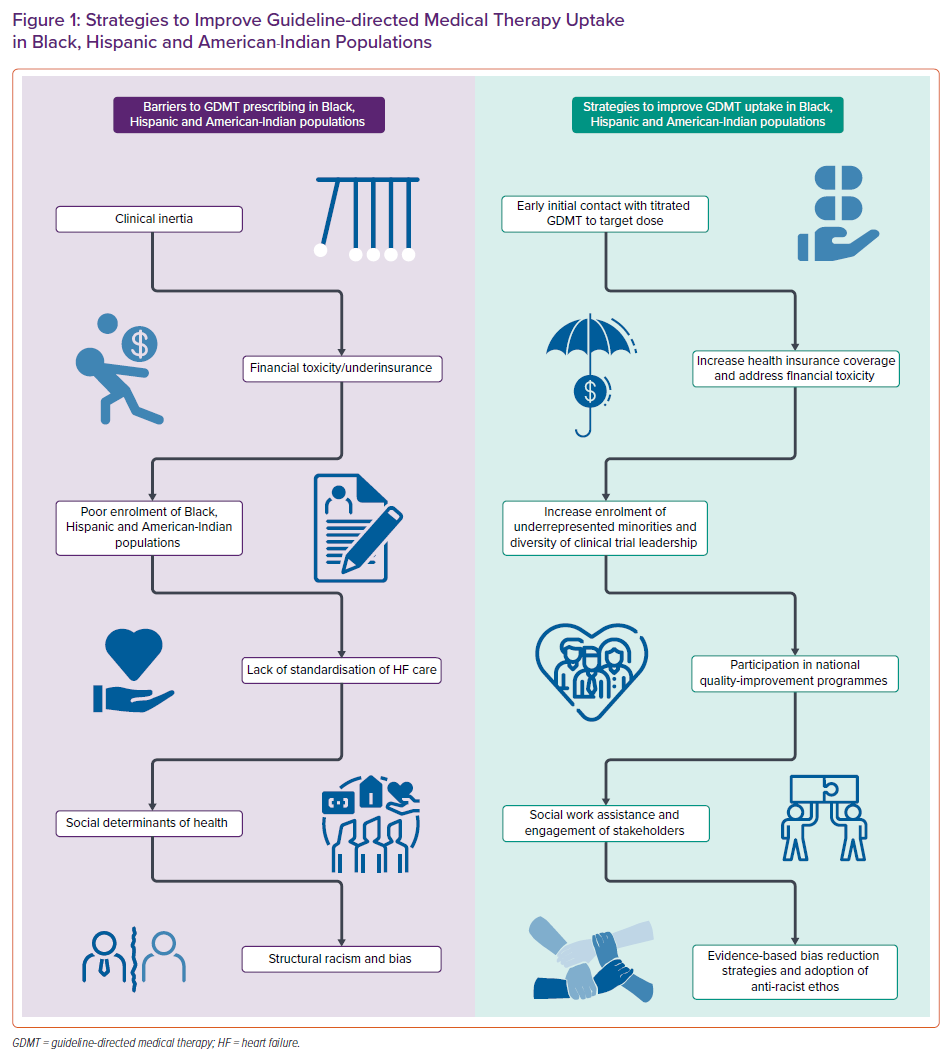
Multiple barriers account for the under-use of GDMT in patients of colour, including clinical inertia, financial toxicity, poor representation in trials, a non-trustworthy medical system, bias and structural racism (Table 1 and Figure 1). Despite clinical practice guidelines, substantial gaps in prescribing GDMT persist. Differential access to lifesaving GDMT for HF serves to worsen HF disparities for people of colour.
Clinical inertia is the lack of treatment intensification in patients not at evidence-based goals of care.26 Black patients and Hispanic patients are less likely to receive GDMT.15,16,22,27 Clinical inertia may be commonly seen in outpatients with HF who may have presumed ‘clinical stability’, thus delaying initiation of GDMT or uptitration to target doses.26 Concerns about Black and Hispanic patients’ ability to afford medications may lead to clinical inertia. A national study revealed that Black and female patients were less likely to be prescribed SGLT2I.28 Clinical inertia contributes to the ‘risk-treatment paradox’ where HF patients at greatest risk of poor outcomes are less likely to receive appropriate therapy.20,29
Financial toxicity refers to the financial strain that patients experience while accessing health care and plays a role in the underuse of GDMT.30 Ethnic minorities are over-represented in lower socio-economic status and wealth inequality has accelerated along racial and ethnic lines.31 Patients of colour are more likely to be paid poverty-level wages than White workers and this leads to inability to access benefits, including health insurance and medication.32 Insurance is necessary for clinic visits and prescription medications and lack of insurance and underinsurance are contributors to racial and ethnic health inequities.33 Newer GDMT has high co-pays and payment assistance programmes are only available for commercially insured patients.34 Addressing financial factors are critical to enable access to newer HF therapies which have a mortality benefit and reduce the risk of hospitalisation.35–37
Black, Hispanic and American-Indian individuals are poorly represented in randomised clinical trials of pharmacotherapies for chronic HFrEF.38 The proportion of Black and Hispanic patients in HF clinical trials appears to be falling despite the increasing ethnic diversity of the US.38 Lack of diversity and cultural competency of trial investigators is a barrier to enrolment of diverse individuals.39 These same populations are underrepresented as clinical trial investigators and leaders.40 There is lack of data on HFrEF GDMT and outcomes and inclusion among American-Indian patients. Lack of racial diversity leads to exclusion and unacceptable implementation of guidelines based on randomised data which exclude vulnerable populations.
Non-trustworthy medical systems, bias and structural racism negatively influences physician decision-making when prescribing GDMT.41 Structural racism refers to “the normalization and legitimization of an array of dynamics – historical, cultural, institutional and interpersonal – that routinely advantage White people while producing cumulative and chronic adverse outcomes for people of color.”42 Racial/ethnic bias negatively affects patient–physician interaction and contributes to adverse outcomes in HF.41 Among patients admitted to an intensive care unit for HF in a national observational study, African-American patients were less likely to receive care by a cardiologist and in this cohort, receiving care by a cardiologist was associated with higher survival for all ethnic groups.43 Clinicians have demonstrated implicit bias in terms of positive attitudes to White patients and negative attitudes towards patients of colour.44 Black and Hispanic patients are more likely to obtain care in the emergency department rather than outpatient settings and to lack access to outpatient care.45
Because of structural racism, Black, Hispanic and American-Indian individuals are more likely to be affected by adverse social determinants of health (SDOH), including low socio-economic status, inadequate social support, reduced access to health care and poor residential environment, which are associated with incident HF through non-traditional mechanisms.7,46 These patients face difficult decisions when the costs of medications and healthcare appointments are at odds with basic food and housing needs, and are at risk for more frequent symptom exacerbation and repeated hospital admissions.47,48 SDOH factors associated with higher HF readmissions include lack of health insurance and income inequality.49 Patients with low socio-economic status are at higher risk of readmission and decreased survival after hospitalisation for HF.50 Low health literacy, more common among Black and Hispanic patients with HF, is predictive of a higher risk of death and hospitalisation.51 Living in a food desert (a low-income area with low access to healthy foods) has also been associated with an increased risk of repeat all-cause and HF-specific hospitalisation.52
Strategies to Improve GDMT in HF for Black, Hispanic and American-Indian Populations
There is an urgent need to develop evidence-based strategies to increase the uptake of GDMT in HF in patients of colour (Table 1 and Figure 1). These strategies if adequately implemented should reduce the HF disease burden in vulnerable populations.
Combating clinical inertia in GDMT prescription can be accomplished by American College of Cardiology/American Heart Association clinical practice guidelines. Initiation of GDMT at first contact regardless of clinical setting can improve outcomes (outpatient or at the time of HHF). Inpatient initiation, continuation and switching of GDMT is associated with improved survival in hospitalised HF patients, and data have shown poor rates of GDMT initiation post-discharge.10,53,54 Intentional uptitration to target doses of GDMT has been associated with improved outcomes. Hispanic patients but not Black patients were more likely to receive all GDMT if they resided in early adopter states of the Affordable Care Act (ACA), regardless of Medicaid Expansion timing, suggesting a cultural/geographical difference in clinician prescribing patterns.55 For Black patients on appropriate GDMT, hydralazine/nitrates should be preferred over soluble guanylate cyclase stimulators as hydralazine/nitrates have shown a mortality benefit in Black patients.12,56
Prioritising patient-centred care is critical in addressing financial toxicity in all patient groups, particularly patients of colour. Financial burden assessment and shared decision-making should include discussions about out-of-pocket costs for brand name GDMT. This may reduce financial toxicity and improve adherence to medications. Adoption of universal health care coverage for historically marginalised populations can address underinsurance and uninsured populations.57. The ACA Medicaid Expansion has been associated with improved access to heart transplants among Black patients.58 Adoption and implementation of health policies (at the federal and state levels) that provide universal health coverage can address underinsurance and lack of health insurance can improve access to GDMT.
Reducing disparities could be achieved via a more diverse enrolment of Black, Hispanic and American-Indian patients in HF trials. Diversifying the leadership of clinical trials to include more women and investigators of colour can diversify trial populations.38,59 Loan forgiveness programmes may improve the diversity of the CV clinical and research workforce.60 Pragmatic clinical trial designs in non-traditional settings, such as churches and barbershops, may aid a diverse recruitment in clinical trials.61 These settings may be more accessible to Black and Hispanic patients and provide clinical trial results that can be easily applicable in real-world and clinical-practice settings. Ensuring that HF clinical trials reflect the ethnic heterogeneity in the US population will lead to more accurate conclusions regarding the efficacy of HF therapies in these populations.38 In addition, race-concordant patient–provider relationships may improve the quality of communication experienced by patients and subsequently adherence.62
There is an urgent need to recognise and address the role of bias and structural racism as it pertains to allocation of HF therapies.63 Sex and racial bias has also been found to influence delayed allocation and inequity in allocation of advanced HF therapies in Black patients.64 Standardised assessments of social factors (e.g. medication adherence and emotional/social support) could reduce disparities.63 Ensuring that HF patients with acute events are admitted to appropriate specialty services with cardiologists regardless of race/ethnicity may also improve outcomes. Engendering an institutional- and policy-wide anti-racist ethos that prioritises learning how to identify, dismantle and replace processes/policies that unfairly disadvantage Black patients will be critical in addressing these systemic biases.
Clinical practice guidelines should consider non-traditional risk factors that influence HF incidence and prevalence, limit the uptake of GDMT in vulnerable minority populations and provide practical recommendations on how to address them.65 This can lead to better standardisation of GDMT prescription across HF populations. It is imperative to increase the participation of hospitals in national quality improvement programmes to help hospitals optimise GDMT use, such as the GWTG-HF programme. A similar programme was able to increase GDMT prescribing to similar or higher levels in African-American patients compared to patients from all other included racial and ethnic groups.19
System-level and multi-level engagement of stakeholders are necessary to eliminate structural racism, physician bias and SDOH that negatively impact GDMT access to patients of colour.65 Stakeholders (patients, healthcare systems/professionals, administrators, community leaders and policy makers) are critical to the development of an implementation plan for equity with measurable benchmarks. Stakeholders can promote policies that ensure the allocation of resources to vulnerable HF patients to counter adverse SDOH. There is an urgent need to make healthcare professionals aware of the existence of structural racism, explicit and implicit bias and its negative impact on healthcare outcomes. Clinicians may benefit from structured implicit bias mitigation training, as well as race, diversity and culture education, since mastery of these competencies may improve physician–patient communication, health literacy, trust and quality of healthcare.66–68
Conclusion
Racial/ethnic groups of colour, particularly Black patients, have the highest burden of HF with higher rates of HHF and overall worse HF outcomes. HF risk remains elevated in Hispanic patients. HF risks in American-Indian patients, although underreported, are likely to be monumental. Ensuring equitable access and appropriate usage of evidence-based GDMT will improve HF outcomes. Multiple reasons exist for GDMT underuse, including system-level factors, such as SDOH, bias and structural racism. Policies and strategies that expand access to health insurance and social resources are critically needed. Evidence-based implicit bias and anti-racism training should be regularly implemented. Implementation research is sorely needed to identify successful mechanisms to actively dismantle and replace policies that contribute to perpetuating structural racism. Increasing diversity in clinical trial leadership and enrolment of historically marginalised ethnic groups for HF trials is needed. Finally, these measures may eliminate barriers to appropriate prescription of GDMT, promote culturally sensitive healthcare and health equity and change outcomes by ensuring optimal management of HF and prevention of adverse outcomes from HF for vulnerable populations.










