While women comprise nearly 50% of US medical school graduates and more than 40% of internal medicine resident physicians, the field of cardiology remains male dominated, with little change in the percentage of women cardiologists over the past 20 years.1 Currently, around one in five general cardiology fellows is a woman. This is comparable to the representation of women in surgical subspecialties, such as thoracic surgery (21%), neurosurgery (17%) and orthopaedic surgery (15%), and highlights the failures to recruit and retain women trainees in cardiovascular medicine, termed the ‘residency to fellowship cliff’.2,3 Beyond the postgraduate medical training period, the percentage of women cardiologists in practice drops to 12.6%.1
Women also hold disproportionately fewer leadership positions within cardiovascular medicine.4 Compared with men, women are significantly less likely to achieve senior academic ranks.5 In a recent analysis of the careers of women physicians in academic medical centres, women were less likely than men to be promoted to associate or full professor or to be appointed as department chairs, and there were no significant changes in these likelihoods over the 35-year study period.6 Unfortunately, the percentage of women cardiologists who experience discrimination in the workplace has not demonstrably decreased in the past two decades. According to serial American College of Cardiology (ACC) Professional Life Surveys, approximately 60–70% of women reported discrimination in professional settings both in 1996 and in 2015.7 This is a significant deterrent for women considering careers in cardiology, and it has secondary impacts on the demographics of the field of heart failure (HF).
Within the subspecialty of advanced HF and transplant cardiology (AHFTC), women have played integral roles in the field’s founding, recognition and development. Yet as with other cardiology subspecialties, women face persistent challenges with respect to achieving pay equity, career advancement and leadership.8 In this review, we discuss the historical representation of women in HF clinical practice, the landscape of women in AHFTC training programmes, factors contributing to sex disparities in clinical practice and HF research, enduring challenges and potential strategies to promote the career development of women in HF.
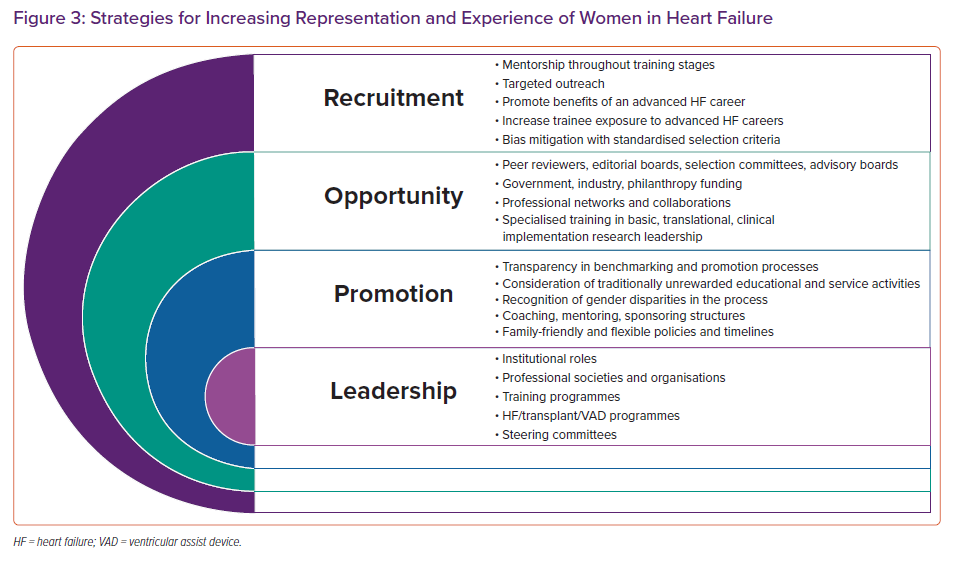
Historical Landscape of Women in Heart Failure
Dr Sharon Hunt is one of the pioneers of the field of advanced HF and cardiac transplantation and is often referred to as the matriarch of heart transplantation.9 Her work at Stanford as a fellow and as faculty during the growth of adult cardiac transplantation in the US set the stage for the inauguration of the field as a subspecialty of cardiology.9 Her clinical and research careers focused on improving the survival of patients after heart transplantation and reducing adverse effects of immunosuppression. In 1976, she reported in Circulation on the outcomes of 109 individuals undergoing heart transplantation at Stanford between January 1968 and August 1976.10 This visionary work was one of the earliest reports suggesting that cardiac transplantation could prolong survival and return patients to improved functional status.10 Dr Hunt was also a leader in major cardiovascular professional societies. She was the Chair of the inaugural ACC/American Heart Association (AHA) Guidelines for the Evaluation and Management of Chronic Heart Failure in the Adult, published in 2001, and served as President of the International Society for Heart and Lung Transplantation from 1995 to 1996.9
Equally important in the field of advanced HF and cardiac transplantation in the 1980s was another trailblazing female clinical investigator, Dr Hannah Valantine. At Stanford, she led innovative research in applying Doppler and M-mode echocardiography to the detection of allograft rejection.11 She was mentored by Dr Hunt, and the two women closely collaborated to advance the science of long-term immunosuppression, cardiac allograft vasculopathy and more.12–15 Dr Valantine was promoted to full professor at Stanford in 2000 and became the inaugural Senior Associate Dean for Diversity and Leadership in 2004.16 She became nationally recognised for her revolutionary success in promoting diversity in the workforce, and was recruited to the National Institutes of Health (NIH) in 2014 as the inaugural Chief Officer for Scientific Workforce Diversity and as a tenured investigator in the National Heart, Lung, and Blood Institute. There, Dr Valantine established novel programmes, such as the Distinguished Scholars Program and the NIH Equity Committee that served to dramatically increase the representation of women, and of African–American/black and Hispanic tenure-track principal investigators, and of women in NIH leadership positions. In addition to each of their remarkable professional legacies, both Dr Hunt and Dr Valantine have inspired generations of clinicians and investigators, many of whom have been women who have subsequently led the field of HF and cardiac transplantation as it continued to evolve in the 1990s.
In 1995, Dr Hunt and others published recommendations on training HF and transplantation in the Journal of the American College of Cardiology. As part of this first Core Cardiology Training Symposium, she and other taskforce members created perhaps the earliest call for a subspecialty in HF and transplantation.17 Dr Hunt wrote:
“For trainees who wish to devote a substantial portion of their career to transplant-related research and patient management, further training beyond other clinical requirements for cardiology training should be required. Although there are currently very few formal training programs in transplant cardiology, a number of centers to provide such training, and an outline of the important aspects can be drawn”.17
The taskforce encouraged such training to occur at centres with established programmes in clinical cardiac transplantation with at least 20 transplant procedures annually. Members emphasised that programmes should be staffed by board-certified cardiologists with expertise in cardiac transplantation, and should require 1 year of training in all phases of pre- and post-transplant clinical management.17
Beginning in 2004, the Heart Failure Society of America (HFSA) built on Dr Hunt’s efforts from the prior decade and began to advocate for the need for a subspecialty focused on advanced HF.18 The HFSA also encouraged other professional societies, such as the ACC, to support its advocacy efforts. The society posited that, in light of an expanding population of individuals with HF, specialists would be uniquely positioned to provide excellence in care for complex patients.
In September 2008, the American Board of Medical Specialties approved a proposal by the American Board of Internal Medicine (ABIM) to establish the subspecialty of Advanced Heart Failure and Transplant Cardiology and a pathway for board certification.19 Since that time, the field of advanced HF has grown significantly and has become a subspecialty that is attractive to women.
Factors Contributing to the Increased Representation of Women in Heart Failure
Dr Hunt postulated that women may be more highly represented in HF for a few reasons, including the enduring presence of women role models and mentors and support for the inclusion of women from the time of the field’s inception.20 It is perhaps the only subspecialty within cardiology that was largely spurred by women and one in which women have played key roles in its development (Figure 1). Dr Hunt also speculated that women have been successful in HF careers because of their proclivity for collaborative work, a particularly important skill for a multidisciplinary field, such as advanced HF and cardiac transplantation.
The field developed with the partnership and leadership of women, and therefore, was not perceived as being “exclusive to male colleagues”.20 Dr Hunt, Dr Valantine and many other renowned and highly accomplished women have advanced the field and served as role models, mentors and sponsors for both women and men.
Women in Contemporary Heart Failure Training and Practice
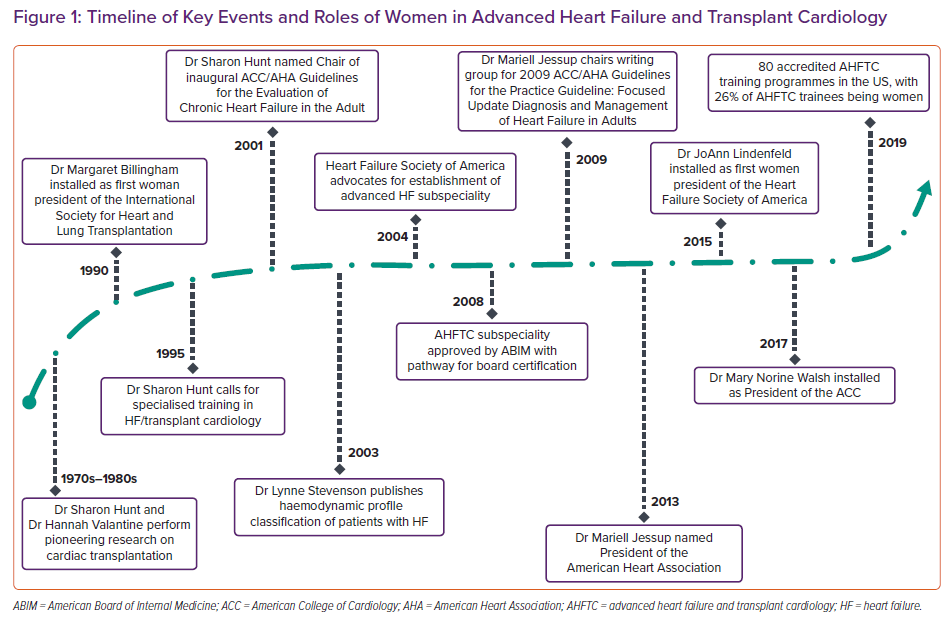
In the US, there are currently 80 accredited advanced HF programmes in 35 states. The ABIM regularly collects data by sex of first-year fellows in Accreditation Council for Graduate Medical Education-accredited training programmes. From 2011 to 2019, the percentage of women in general cardiology fellowship training programmes has increased from 21% to 25%. For women in AHFTC programmes, the percentage is between 26% and 36% (Figure 2). This is significantly higher than that of women in more procedural subspecialties, such as clinical cardiac electrophysiology and interventional cardiology, similar to the trends observed in the demographics of board-certified cardiologists.21
As of December 2016, there were 939 cardiologists who were ABIM board certified in AHFTC; of these, 239 (25.5%) were women.1 Notably, this is compared to only 4.9% women among board-certified interventional cardiologists, 8.6% among board-certified electrophysiologists and 12.5% among board-certified clinical cardiologists.1
In Europe, interest in AHFTC has also continued to grow. According to the European Society of Cardiology (ESC) membership database, as of December 2018, 33.7% of ESC members were women and 33.8% of members of the Heart Failure Association of the ESC were women.22 At the ESC Heart Failure Congress in recent years, the proportion of women attendees has been consistently higher than that of men among the younger age groups. Similar trends have also been seen in the distribution of men and women taking the Heart Failure Association Certification exam in Europe, suggesting increasing interest in HF as a subspecialty among young women cardiologists.22
Within the HFSA, data show that 59% of active members, as of November 2020, were women (J Leonard, Personal Communication, 20 November 2020). However, only 29% of the women members are physicians and 9% are trainees. Of the women members, 32% are early career (0–5 years after training), 26% mid-career and 36% established career (6% did not indicate a career level).
Women in Leadership Positions in Heart Failure
Despite the relatively higher proportions of women in HF, their representation in professional society leadership positions remains low. The AHA was founded in 1924, and Dr Helen Taussig served as its first woman president in 1965.
Among subsequent women AHA presidents was Dr Mariell Jessup (President 2013–2014), who was also instrumental in achieving formal recognition for AHFTC as a certified subspecialty.23 Additionally, she chaired the writing group for the 2009 Focused Update: ACC Foundation/AHA Guidelines for the Practice Guideline: Focused Update Diagnosis and Management of Heart Failure in Adults, served as vice chair of the writing committee for the 2013 ACC Foundation/AHA Guideline for the Management of Heart Failure and vice chair of the writing committee for the 2017 ACC Foundation/AHA/HFSA Focused Update of the 2013 ACC Foundation/AHA Guideline for the Management of Heart Failure.24–26
Since the founding of the ACC in 1949, there have been 68 organisational presidents; four of these have been women.27 Of these women, one, Dr Mary Norine Walsh (President 2017–2018), practices in advanced HF and cardiac transplantation. In Canada, HF clinician, Dr Heather Ross, has served as President of both the Canadian Society of Transplantation (2004–2005) and the Canadian Cardiovascular Society (2015–2016).28,29 The Heart Failure Association of the ESC was launched in 2004 and has not been led by a woman to date.30
Since 1996, there have been 15 presidents of the HFSA. The first woman HFSA President, Dr JoAnn Lindenfeld, was inaugurated in 2014, nearly 10 years after the organisation’s founding. Dr Biykem Bozkurt (President 2019–2020) and Dr Nancy Albert (President 2020–2021) are the organisation’s second and third women presidents, respectively. Similarly, from 1981 to 2020, there have been 37 presidents of the International Society for Heart and Lung Transplantation. Of these, only five (13.5%) have been women.31 One of these five women, Dr Maryl R Johnson, also served as President of the American Society of Transplantation (2010–2011).32
Women and Discrimination in Heart Failure Clinical Practice and Research
Despite the demographics of women in HF clinical practice, women still perceive sex-based imbalances with regard to salary, leadership positions and academic promotions.8 In 2019, Moayedi and colleagues surveyed 236 international HF cardiologists to determine factors that influenced their career choices.8
Among both women and men, the three most important factors attracting respondents to careers in HF cardiology included patient complexity and continuity of care, clinical diversity and evolving technology. There were no differences in rank order by sex of the respondent.8 Participants emphasised an increased need for sponsorship, increased support for maternity leave and income transparency to attract and maintain women in HF.8
Regarding academic rank, more men than women had achieved the rank of professor with no differences at the assistant or associate professor levels.33 While this is a potentially biased sample of those who responded to a voluntary survey, these findings are consistent with disparities observed in academic medicine, at least in the US, more broadly.6
Women also remain underrepresented as clinical trialists in cardiology and in HF. We previously reviewed the publications referenced in Class I recommendations in both US and European guidelines for management of HF, as well as all HF clinical trials published from 2001 to 2016 with more than 400 participants.34 The overall proportions of women as first authors in the referenced publications in the US and European guidelines were 18% and 16%, respectively, and, as senior authors, were 13% and 12%. Of the examined clinical trials, 16% of publications had a woman as first or senior author, and the median number of women authors per trial was one. Overall proportions of women as first or senior authors of HF clinical trial publications did not increase over the 15-year study period.
Industry-funded trials had fewer women authors per trial; it has been previously demonstrated that women receive fewer total dollars from financial relationships with pharmaceutical and device companies compared with men.35 In addition, we found an association between the number of women authors of HF clinical trials with the enrolment of women participants.34 Outreach initiatives and dedicated efforts are needed to increase support for women HF researchers and site investigators, as well as collaborations with industry, which may also help stimulate increased representation of women in HF clinical trials.
Another recent systematic review of 403 HF randomised controlled trials published in high impact journals from 2000 to 2019 found that women only represented 15.6% of lead authors, 12.9% of senior authors and 11.4% of corresponding authors.36 Notably, there were no significant changes in the representation of women as lead authors over time. Women were less likely to be lead authors in multicentre trials, those conducted in North America or Europe or had men as senior authors.36
Reconciling Sex Disparities in Heart Failure Practice and Research
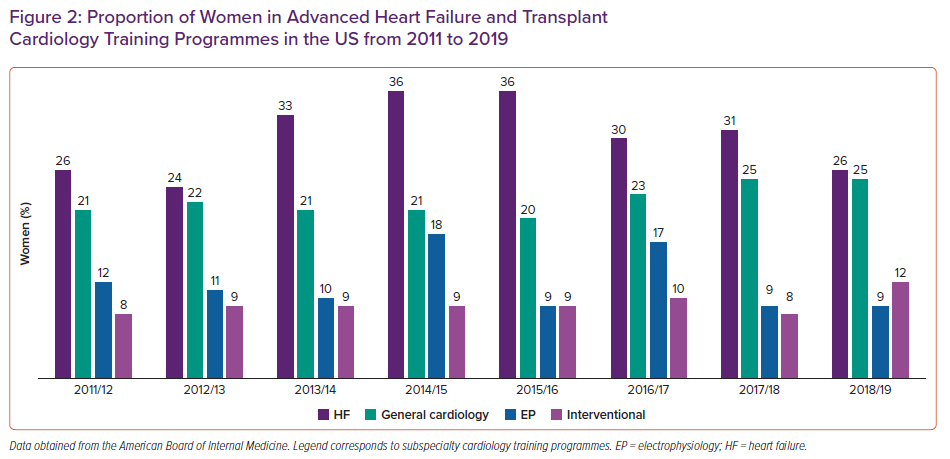
These data highlight the critical need to sustainably increase and advance diversity, equity and inclusion in the field of AHFTC. In 2019, Dr Nancy Sweitzer proposed a valuable multipronged thematic framework to address these issues.33 AHFTC can be an emotionally demanding specialty that frequently encompasses advanced and critical illness, death and dying. This can be burdensome to both men and women, but can be exacerbated by lack of institutional support or mentorship, which may disproportionately affect women. As Sweitzer writes: “workplace discrimination is not merely an issue of numbers”, and culture change must be implemented to reduce workplace harassment and microaggressions.33 While equal hiring, remuneration and representation of women in HF is paramount, we also need to strive for policies that lead to lasting behavioural, cultural and structural changes. These actions are especially important to advance women’s research careers and include the diversification of manuscript and grant reviewers, journal editorial boards and steering and leadership committees.37 Equally important strategies include the implementation of family-friendly policies, flexible work structures and support for adequate and equitable parental leaves. Additionally, sponsorship is necessary for creating diverse professional networks and workplace paradigms that value and reward mutual respect, teamwork and collaboration (Figure 3).
Conclusion
Since its inception, the field of advanced HF and cardiac transplantation has had pioneering women cardiologists at its helm. These women have helped to define the subspecialty and served as role models, mentors and sponsors for many generations of female and male HF physicians. The relatively increased representation of women in HF training programmes and clinical practice may uniquely position us to provide guidance to other subspecialties with respect to the recruitment and promotion of women. However, the small numbers of women in leadership positions in clinical practice, academics and research, and enduring disparities, highlight that many opportunities for improvement remain, and undoubtedly women in HF will continue to lead the way.